- TRENDING
- Lok Sabha Elections
- Mera Power Vote
- Nagaland Board Result
- IPL 2024
- Live Election News
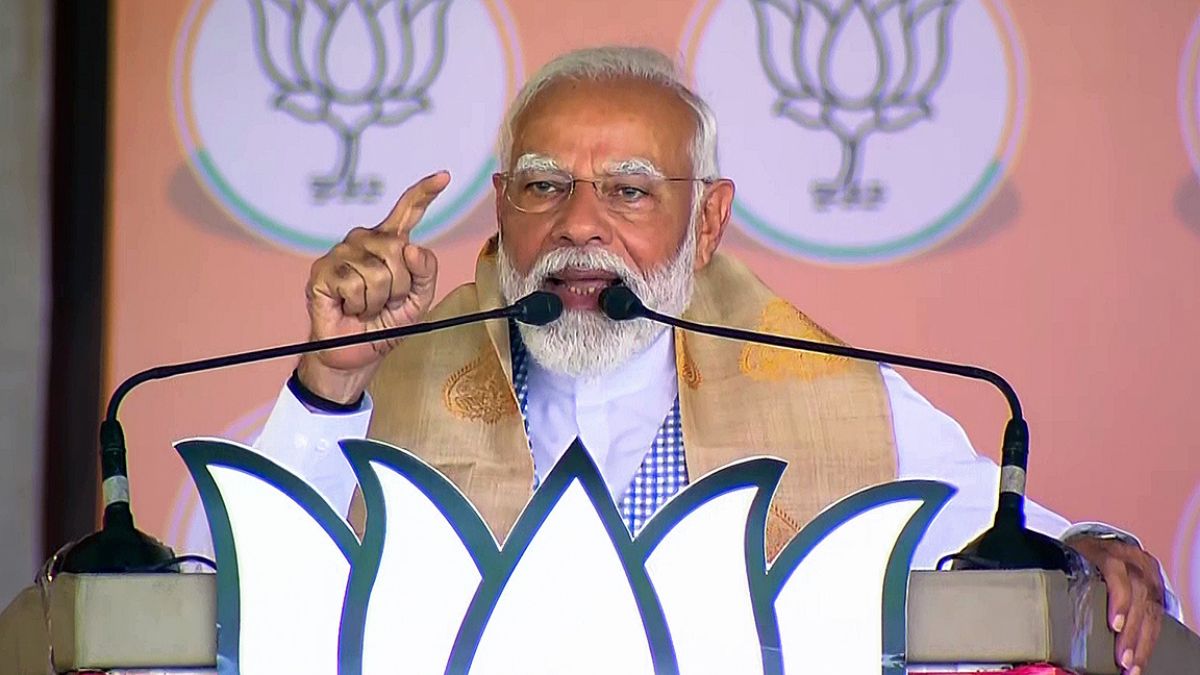
- PM Modi
- Ott Releases
- BTS
- CBSE Result
- 18 minutes agoLifestyle
- 31 minutes agoLifestyle
How To Keep Your Makeup Flawless Despite The Summer Sweat? Expert Weighs In
- 1 hour agoLifestyle
20 Powerful Quotes By BLACKPINK To Make You Feel Worthy And Special
- 11 minutes agoEntertainment
- 1 hour agoEntertainment
Rekha Kisses Richa Chadha's Baby Bump At Heeramandi Premiere, Watch Viral Video
- 18 minutes agoBusiness
Tech Mahindra Shares Rise Over 12% After Q4 Results; Company To Consider Dividend
- 2 hours agoTechnology
Lava Prowatch ZN And Prowatch VN Sale Starts Today: Check Specs, Special Prices Here